Don’t overlook any of your client’s injuries
Common, uncommon and commonly overlooked injuries in car crashes
Every crash is different. People are different and have different experiences, thresholds, and susceptibilities. Someone reviewing the “file” instead of taking a deep dive into the event, person, and data may try to tell you otherwise. Don’t let them.
Consider the lens through which you are reviewing the range of injuries associated with your client’s trauma, specific to orthopedic injuries, in this instance a motor-vehicle crash. Specifically, evaluate the injuries your client sustained, including primary injuries and associated injuries. Make sure to read between the lines, listen to your client, and listen to their treating doctors to help put their life back together. That is your job as their personal injury lawyer.
Many times, clients come in and complain of pain – “My neck is sore and achy…it hurts when I…” or “I can’t…my back feels like it is on fire…” Neck and back injuries are the most common injuries associated with a motor-vehicle crash. There are many types of common neck and back injuries after a motor vehicle crash including:
Facet joint syndrome
While being very common, there are instances where someone is complaining of pain, yet MRI imaging does not show a disc injury. Instead, the culprit can likely be facet joint pain and you may not even see it on the imaging.
The facet joints are the lateral joints in the spine that connect the vertebrae together. They are lined with cartilage and help promote healthy movement of the spine. They can be damaged through normal aging or through a traumatic injury, causing pain or facet joint syndrome.
How is facet joint syndrome diagnosed?
A practitioner knowledgeable in spinal disorders will take a history, perform a physical exam, and review imaging. Depending on various factors, including technique and equipment, it is often the case that this injury is not identified on even advanced imaging. The classic finding of facet syndrome is pain and tenderness over the facet joints with extension (bending backwards).
How is facet joint syndrome treated?
A conservative nonoperative approach is generally utilized to manage the pain and improve the function for these injuries. This treatment plan can include physical therapy, anti-inflammatory medications, and strengthening exercises. In addition, minimally invasive therapies such as injections for diagnosis and treatment may be used.
Intraarticular injections involving steroids help reduce pain and inflammation. Medial-branch blocks use anesthetic agents on the nerves that arise from the facet joints. If the pain is relieved by these blocks, it is a good sign that a radiofrequency ablation may provide longer-lasting relief. This is accomplished by heating the nerves of the facet joints to burn them off. This can provide pain relief from six months to two years. The bad news is that the nerves grow back and will likely need to be addressed in the future if your client is fortunate enough to find relief. (Patel T. Watterson C. McKenzie-Brown AM, Spektor B, Egan K, Boorman D. Lumbar Spondylolisthesis Progression: What is the Effect of Lumbar Medial Branch Nerve Radiofrequency Ablation on Lumbar Spondylolisthesis Pregrssion? A Single-Center, Observational Study. J Pain Res. 2021; 14:1193-1200. See also Conger A. Burnham T, Salazar F, Tate Q, Golish M, Petersen R, Cunningham S, Teramoto M, Kendall R, McCormick ZL. The Effectiveness of Radiofrequency Ablation of Medial Branch Nerves for Chronic Lumbar Facet Joint Syndrome in Patients Select by Guideline-Concordant Dual Comparartive Medial Branch Blocks. Pain Med. 2020 May 1;21(5):902-909.)
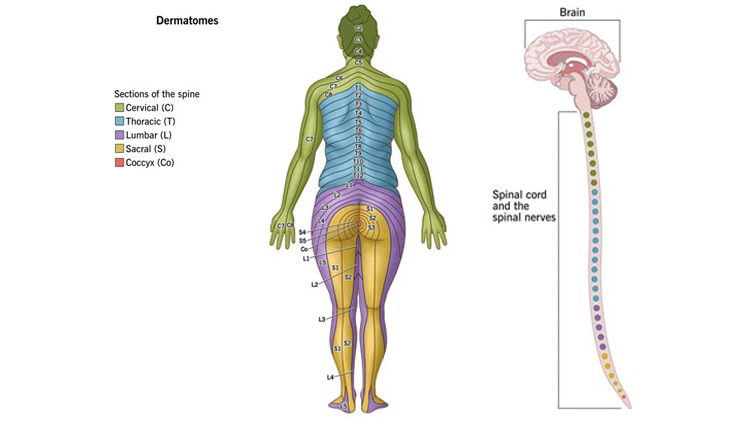
Radiating pain
This condition is an irritation or compression of one or more nerve roots in the spine. General patterns exist which can assist in correlating the symptom to the injury. These patterns are often referred to as dermatomes.
Causes
Herniated disc: a rupture in the fibrous outer wall of a vertebral disc, which allows the soft nucleus of the disc to bulge outward. This bulge can press harmfully against a nerve root. When a spinal disc weakens, it allows vertebral bones above and below the disc to shift out of position, which can happen over time or in an instant, and can pinch or impinge nearby nerve roots.
Symptoms
Symptoms may include pain, weakness, numbness, and tingling, and may vary depending on the level of the injury.
(See Gupta A, Upadhyaya S, Yeung CM, et al. Does Size Matter? An Analysis of the Effect of Lumbar Disc Herniation Size on the Success of Nonoperative Treatment. Global Spine Journal. 2020;10(7):881-887. Weinstein JN, Tosteson TD, Lurie JD, et al. See also:
Surgical vs Nonoperative Treatment for Lumbar Disk Herniation: The Spine Patient Outcomes Research Trial (SPORT): A Randomized Trial. JAMA. 2006; 296(20):2441-2450. See also: Gugliotta M, da Costa BR, Dabis E, et al. Surgical versus conservative treatment for lumbar disc herniation: a prospective cohort study. BMJ Open 2016;6:e012938 Lin JH, Chiang YH, Chen CC. Lumbar radiculopathy and its neurobiological basis. World J Anesthesiol 2014; 3(2): 162-173.)
Spinal stenosis
Spinal stenosis is a narrowing of the spaces within your spine, which can put pressure on the nerves that travel through the spine. This occurs most commonly in the neck and low back. Some people may not experience any symptoms, whereas others may have pain, numbness, tingling, and/or muscle weakness. Spinal stenosis is commonly caused by herniated or bulging discs.
Spinal stenosis is often diagnosed through MRI and CT scan. In-office nerve testing may help determine the health of the nerves affected by the stenosis. Treatment options may include medication, physical therapy, and injection therapy, such as epidural steroid injections. If the stenosis is severe enough, or other treatment options fail, surgery may be indicated. (Prevalence of lumbar spinal stenosis in general and clinical populations: a systematic review and meta- analysis. European Spine Journal. 2020. See also Objective measurement of free-living physical activity (performance) in lumbar spinal stenosis: are physical activity guidelines being met? The Spine Journal. 2017. 3. Cost-effectiveness and Safety of Interspinous Process Decompression (Superion). Pain Medicine. 2019.)
Commonly overlooked injuries
You are going to be presenting substantially fewer injuries at trial (or even in a demand package) than your client may have presented with after the crash. This is because your client will go through a rehabilitation phase after the crash with the hopes of getting better. Some, most, or even all of the initial complaints may subside or even resolve while the injured person is taking time away to rest, to not work, to get the medical care that has been recommended and which they need.
Often the objective findings demonstrate anatomical changes. In good situations, the person is “feeling better” or has “good days and bad days” but is not at their pre-crash condition, nor is performing the same activities to the same degree. The ability to cope is not as strong, they do not bounce back like they used to, they “feel older” after the crash. The road ahead can be long and will often include chronic pain and various treatment modalities. Consider the constellation of symptoms associated with the event. Most medical professionals will agree that six months of time is sufficient to classify the pain as chronic.
According to the National Library of Medicine, chronic pain is a leading chief complaint in an adult ambulatory care setting. Patients should be evaluated for the nature of their pain both physically and psychologically in addition to how pain has affected every aspect of life. The treatment goal of chronic noncancer pain (CNCP) is to improve function; therefore, setting expectations and providing education surrounding techniques to decrease pain intensity and frequency of flares to improve quality of life. (https://www.ncbi.nlm.nih.gov/books/NBK470523/)
(Borsook D, Youssef AM, Simons L, Elman I, Eccleston C. When pain gets stuck: the evolution of pain chronification and treatment resistance. Pain. 2018;159(12):2421-2436. See also Morlion B, Coluzzi F, Aldington D, Kocot-Kepska M, Pergolizzi J, Mangas AC, Ahlbeck K, Kalso E. Pain chronification: what should a non-pain medicine specialist know? Curr Med Res Opin. 2018 Jul;34(7):1169-1178. 4. International Association for the Study of Pain)
Distracting injury
Some injuries can be overlooked or overshadowed by another more prominent or obvious injury. A distracting injury has been defined as any injury that distracts the patient’s attention from another separate injury, including the vertebral spine. In such a case, you may have a person who was involved in a lateral impact/T-bone type impact, causing the driver, Plaintiff, to smash their shoulder and body towards their door, causing damage. While biomechanics need to be examined, it may be the case that an obviously injured shoulder may distract from a related neck injury or inter-ear (labyrinthine) concussion caused by the same mechanism of injury.
The primary injury or injuries or chief complaint(s) may stay the same, but often there is variance. These are people, not files. We need to consider things like adrenaline, epidemiology, distracting injuries, life experiences, and the facts surrounding the actual medical evaluation at the time.
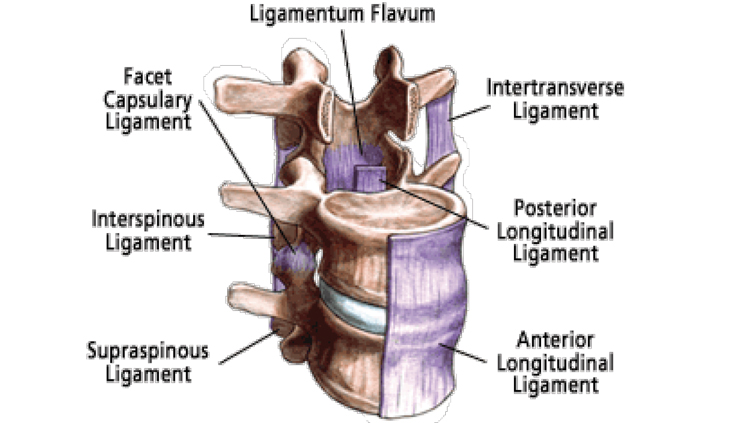
Ligaments in the spine
The three most important ligaments in the spine are the Ligamentum Flavum, Anterior Longitudinal Ligament, and the Posterior Longitudinal Ligament:
1. The Ligamentum Flavum covers the dura mater which is the layer of tissue that protects the spinal cord. This ligament connects the facet joints to create a small covering over the posterior openings between the vertebrae.
2. The Anterior Longitudinal Ligament connects the front of each vertebra to each other. This ligament runs up and down the spine.
3. The Posterior Longitudinal Ligament extends up and down behind the spine and inside the spinal canal.
After a traumatic injury, the ligaments in the spine can become injured, creating symptoms including buckling, inflammation, instability due to becoming overstretched or contorted. These can be permanent, painful, and debilitating injuries. Surgical consultation may be required.
(ISIS Practice Guidelines for Spinal Diagnostic and Treatment Procedures: 2nd Edition. Nikolai Bogduk. Atlas of Image-Guided Spinal Procedures. Michael Furman. Danne Miller board review series.)
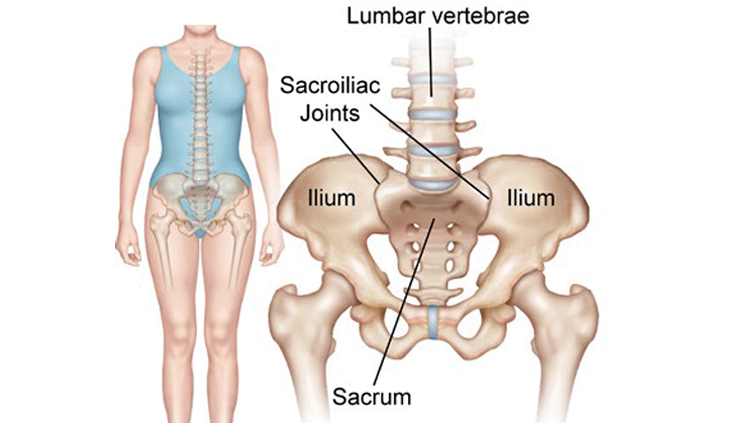
Sacroiliac joint dysfunction (SI joint pain)
The sacroiliac joint lies next to the bottom of the spine, below the lumbar spine and above the tailbone (coccyx). It connects the sacrum (the triangular bone at the bottom of the spine) with the pelvis (iliac crest). (https://cedars-sinai.org/health-library/diseases-and-conditions/s/sacroiliac-joint-dysfunction.html)
Dysfunction in the sacroiliac joint can cause low-back pain and/or leg pain as well as instability. The leg pain can be particularly difficult and may feel similar to sciatica or pain caused by a lumbar disc herniation. The most common symptoms for patients are lower back pain and the following sensations in the lower extremity: pain, numbness, tingling, weakness, pelvis/buttock pain, hip/groin pain, feeling of leg instability (buckling, giving way), disturbed sleep patterns, disturbed sitting patterns (unable to sit for long periods, sitting on one side), pain going from sitting to standing. (https://cedars-sinai.org/health-library/diseases-and-conditions/s/sacroiliac-joint-dysfunction.html)
Chronic SI joint pain is relatively common, accounting as a significant contributor in an estimated 10-38% of cases of chronic low-back pain. Physical examination is performed to isolate and identify SI joint pain, but can result in false positives and false negatives, including on each side. Accurately diagnosing sacroiliac joint dysfunction can be difficult because the symptoms mimic other common conditions, including other mechanical back pain conditions like facet syndrome and lumbar spine conditions including disc herniation and radiculopathy (pain along the sciatic nerve that radiates down the leg). A diagnosis is usually arrived at through physical examination (eliminating other causes) and/or an injection (utilized to block the pain). https://cedars-sinai.org/health-library/diseases-and-conditions/s/sacroiliac- joint-dysfunction.html)
If not utilizing diagnostic injections, it is encouraged that a practitioner’s examination includes five provocative maneuvers, with at least three positive tests, including at least one being the thigh thrust or compression test. These tests, while simple, are inconsistent among practitioners and can be unreliable.
A recent article titled A Review and Algorithm in the Diagnosis and Treatment of Sacroiliac Joint Pain, works to clarify the approach to diagnose and treat SI joint pain. This review article highlights the importance of optimizing the diagnosis as soon as possible to guide treatment. Image-guided injection remains the gold standard for the diagnosis of SI joint pain. (See Falowski S, Sayed D, Pope J, Patterson D, Fishman M, Gupta M, Mehta P. A Review and Algorithm in the Diagnosis and Treatment of Sacroiliac Joint Pain. J Pain Res. 2020;13:3337-3348. See also Wallace P, Bezjian Wallace L, Tamura S, et al. Effectiveness of Ultrasound-Guided Platelet- Rich Plasma Injections in Relieving Sacroiliac Joint Dysfunction. American Journal of Physical Medicine & Rehabilitation. 2020 Aug; 99(8):689-693.)
Curvature and shape of the spine
Various conditions exist, some of which are detailed below. Most of these are often overlooked unless and until reviewed by a surgeon, often years after the crash.
Spondylolisthesis
Spondylolisthesis is a spinal condition in which the vertebrae may slip forward or backward. A forward slip of the vertebrae is called anterolisthesis. A backward slip of the vertebrae is called retrolisthesis. This altered positioning of the vertebrae may cause compression of the nerves down the central spinal canal as well as the nerve openings on each side of the vertebrae.
Spondylolisthesis may occur as a result of a weakened or damaged disc, including the areas around the disc. Aging of the disc, traumatic injury, compression fracture, overuse injury or birth defect, along with tumors, can also cause an altered positioning of the vertebrae making a person either have slippage or experience it in certain positions.
Some people may not experience pain. Other people may have pain in their neck, mid back or lower back along with pain, numbness or weakness that occurs in the arms, hands, legs or feet.
Imaging the spine is helpful with this diagnosis. X-rays may be taken in the form of flexion and extension views to evaluate the degree of severity. An MRI of the spine may be obtained for further evaluation and comparison imaging can be utilized to evaluate the progressive nature and impact of the condition.
Physical therapy may be helpful with strengthening and stretching exercises of the neck and lower back. Temporary use of a neck or a back brace may be helpful for flareups of pain along with rest, ice and anti-inflammatory medications may be helpful to reduce inflammation and pain symptoms. None of these will fix the problem, however.
Surgical consultation is helpful at times to determine the severity of the vertebral movement. For more mild cases, spinal injection therapies such as epidural steroid injections and facet-joint injections can be done to improve symptoms as well as reduce inflammation irritating the structures of the spine. Radiofrequency ablation of the sensory nerves from the joints of the vertebrae can be helpful to reduce symptoms for several months or years. Surgery may be needed if these modalities are not effective. Surgery can be done to remove the pressure around the nerves in the spine. If the spine is considered to be unstable, then surgery may be required in the form of a fusion to stabilize the structures of the spine.
Spinal instability
Spinal instability describes a greater- than-normal range of motion between two vertebrae, resulting from a disc’s deterioration to the point that it becomes unable to support the weight of the body through that portion of the spine.
Dynamic instability
Dynamic instability is a type of spinal instability that occurs when the spine is unable to maintain its normal alignment and movement during common movements and activities, like bending or walking.
Static instability
Static instability can occur when the spine cannot maintain its normal alignment when the body is at rest.
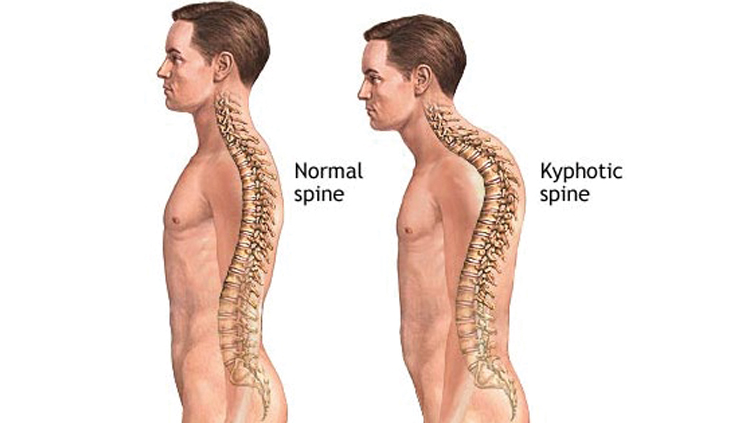
Kyphosis
Kyphosis is an exaggerated, forward rounding of the upper back.
Kyphosis is associated with weakened back muscles and difficulty doing tasks such as walking and getting out of chairs. The spinal curvature can also make it difficult to gaze upward or drive and can cause pain when you lie down.
(https://www.mayoclinic.org/diseases-conditions/kyphosis/symptoms-causes/syc-20374205)
This will impact activities of daily living, quality of life and functionality.
Conclusion
Pain is different from person to person, from time of day, from action to action. Your client’s injuries on paper may seem one way but the effect they have on the person is what matters. The question you need to ask yourself is how your client’s life is impacted. One of the best ways to do this is to communicate with your client, review the medical treatment, records and compare them.
In my experience, asking questions of doctors under oath, it is quite rare for a patient to come in and say that they have instability due to their SI joint, or hypertrophy in their facets, or inflammation in their ligamentum flavum. This is why it is our job as the lawyer to help identify the puzzle pieces and assist our client in communicating these issues to their medical providers. We are not responsible for their bodies; that is between the medical professionals and your client. We, as the lawyer, the counselor, guide and advocate, are responsible for preparing and presenting their case and putting their life back together.
As you navigate your client’s life story and injury claim, review the medical records carefully and really listen to your client. You may find that they continue to have complaints and are experiencing injuries beyond the common ones, do not overlook these and you will be equipped to protect them.
Alex Zeesman

Alex Zeesman is a founding partner of Accident Fighters, APC. Mr. Zeesman handles all aspects of personal injury matters. He received his Juris Doctor degree from the University of the Pacific, McGeorge School of Law.
Copyright ©
2026
by the author.
For reprint permission, contact the publisher: Advocate Magazine