Powerful ways to prove your client’s brain injury objectively
Don’t just defend the “subjective” evidence of a brain injury, use state-of-the- art multi-disciplinary “objective” evidence to prove your client’s brain injury
Your client has a brain injury. You know it. The defense knows it. So, what will the defense say to raise doubt in the jurors’ minds and to avoid taking responsibility? One standard defense argument is that all evidence of your client’s injury is “subjective” and based on self-reports to treating doctors. The defendant will likely claim that your client’s symptoms are caused by something else (anything but a TBI). Alternatively, the defense may admit your client was injured, but will claim your client has fully recovered or has minimal limitations.
While subjective evidence is used every day by treating physicians and has solid evidentiary value, it is possible to take the defense argument head-on and to “objectively” demonstrate your client’s brain injury with overwhelming evidence from multiple objective tests. These tests will provide measurable objective data about your client’s brain that your client cannot control or manipulate. You can then argue the odds are astronomical that these diverse tests all pointing to the same brain-injury conclusion are somehow mistaken. At the same time, these tests may also show the full extent of your client’s impaired cognition and functioning, adding case-changing elements to your client’s life-care plan.
These objective tests, further described below, include advanced radiologic techniques that go far beyond the standard MRI or CT scan, including volumetric scans measuring brain atrophy, perfusion scans measuring decreased blood flow, fMRI scans measuring decreased blood flood during cognitive processes, DTI scans measuring impaired nerve signal transmission, SWI scans that detect subtle microbleeds, MRS scans measuring abnormal metabolite ratios, PET scans measuring impaired glucose/energy uptake, SPECT scans creating 3-D models of impaired blood flow, as well as auto-antibodies blood tests, neuroendocrine blood tests, neuro-optometric testing, vestibular and balance testing, and neuropsychological and speech pathology testing.
These tests can be used for both traumatic brain injuries and for toxic brain injuries such as carbon monoxide poisoning, chemical exposure, and other toxic tort matters.
Beyond the standard MRI and CT
An injured brain may appear normal on a conventional 1.5 Tesla MRI or CT scan because these scans are not sensitive to detecting diffuse axonal injuries that may substantially impair cognition and function. However, there are many other powerful radiologic tools to objectively prove your client’s brain injury.
While the standard 1.5 Tesla MRI can be thought of as a microscope to image small structures of the brain, the 3.0 Tesla MRI has twice the magnetic field strength, substantially increasing image resolution and potentially identifying injuries that a 1.5 Tesla MRI would miss. Other factors in how the scans are performed may also affect the ability of the scan to detect injury, including how thick or thin the imaged slices are (thinner slices up to 1 mm are preferred over slices every 5 mm to avoid missing injuries), and scanning multiple planes of the brain (i.e., the x, y, and z axis planes, or the sagittal, coronal, and transverse planes, respectively). Furthermore, an injury that is detected on multiple planes will rebut standard defense claims that the injury finding is an alleged “artifact” from the scan and not a real injury.
Volumetric brain measurement scans
When the brain is exposed to trauma or injury, all or certain structures of the brain may atrophy or shrink. Volumetric MRI brain measurements are used to measure the volume of specific structures in the brain. Brain atrophy can be detected by comparing the client’s brain to standard norms for the client’s demographic or by successive MRIs over time showing abnormal volume loss of your client’s brain or its structures. This can be shown by both visual size comparisons and objective volume data reflecting the percentage of atrophy.
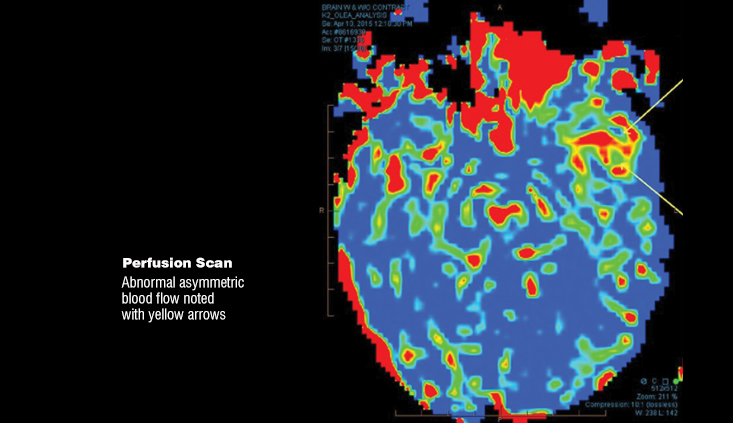
MRI perfusion scans
Injured areas of the brain may have reduced blood flow. An MRI perfusion scan measures blood flow in the brain using a contrast agent that is injected into the client’s bloodstream, creating a visual multi-colored representation of reduced blood flow to injured areas of the brain. Differences in blood flow between a non-injured hemisphere and an injured hemisphere of the brain can be made readily apparent to jurors.
Functional MRI scans (fMRI)
Similarly, injured areas of the brain may have reduced blood flow that becomes apparent when performing certain cognitive tasks. An fMRI measures blood flow in the brain while it is actively functioning, for example, processing sounds that may be played, observing visual scenes that may be presented, or performing small motor movements. fMRI can detect signal changes as small as 1%, making it possible to detect subtle changes in brain activity as a result of TBI.
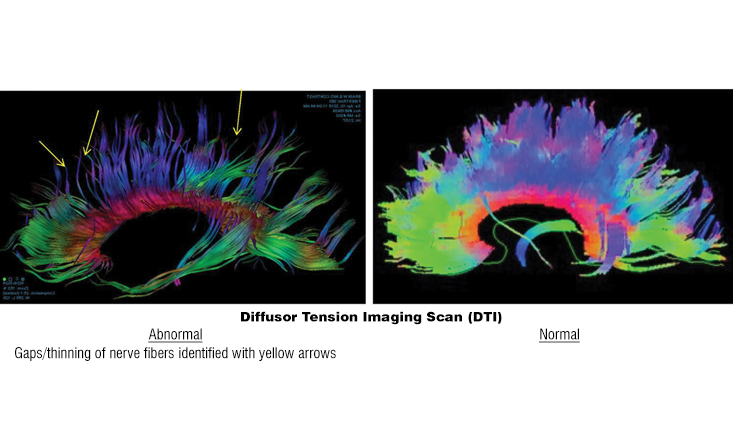
Diffusor tensor imaging scans (DTI)
Brain injuries may impair the ability of the axons in the brain to effectively transmit messages. DTI isolates water movement along white matter containing nerve fibers (axons) within the brain, and measures whether the water molecules in the axons are flowing properly along axonal directions. The DTI scan depicts white matter pathways as multicolored fibers, and if the scan identifies water flows that are slowed or blocked due to brain injury, gaps or thinning in these multicolored fibers may be visible.
Susceptibility-weighted imaging scans (SWI)
Brain injuries with diffuse axonal injury are often associated with microbleeds in the deep brain that are not routinely visible on conventional CT or MRI. SWI is a type of MRI sensitive to blood products that makes visualization of microbleeds as dark spots on the scan significantly more apparent.
Magnetic resonance spectroscopy scans (MRS)
Brain injury may cause abnormal ratios of metabolites in the brain. MRS uses MRI physics at the cellular level to measure the ratios of various metabolites in the brain, including myoinositol, choline, creatine, N-acetylaspartate, and lipids. A visual representation of this abnormality can be seen in a graph depicting those ratios that violate the “Hunter’s Angle” of a normal brain scan.
Positron emission tomography scans (PET)
Brain injuries can impair the brain’s ability to process energy (glucose) in affected areas. PET scans produce a 3-D image of functional glucose metabolism in the brain using a radioactive glucose tracer injected into the bloodstream. As the glucose is metabolized in the brain (relatively slower in injured areas compared to other standardized norms), the areas of brain injury can be visualized with contrasting colors for the jury.
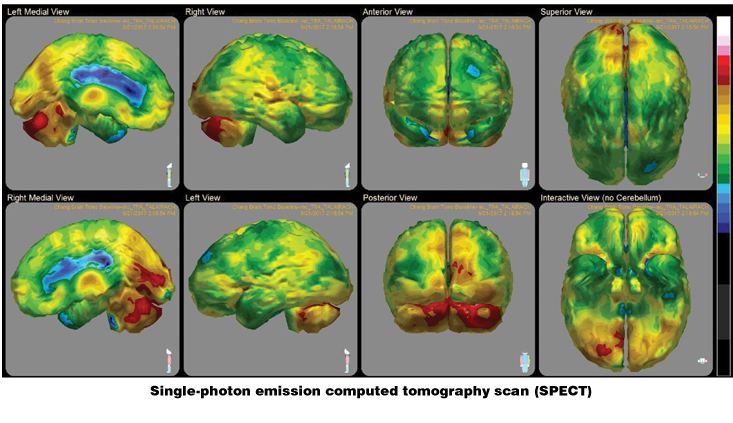
Single-photon emission computed tomography scans (SPECT)
Similarly, SPECT scans also use radioactive tracers to produce a 3-D image, but instead measure blood flow rather than glucose uptake, with brain-injured areas visualized through less blood flow in contrasting colors in the injured area. SPECT scans may not be as detailed as PET scans, but SPECT scans are also not as expensive as PET scans.
Auto-antibodies blood tests
Following brain injury (including by trauma or toxins), neuron- and glial-specific proteins are released into circulation through the damaged blood brain barrier. Released neuronal and glial elements accumulate and stimulate B lymphocytes to produce autoantibodies that are reactive against these proteins. Increased autoantibodies against brain-specific proteins in blood samples are an indication of neuronal damage. Your client’s levels of these autoantibodies can be measured against standardized norms to visually and graphically demonstrate the brain injury.
Neuroendocrine blood tests
The pituitary gland is a small gland located at the base of the brain that is responsible for the production of hormones that play an important role in many different bodily functions, including growth, development, reproduction, and metabolism. The pituitary gland can be damaged by a brain injury, which can in turn impair production of key hormones such as growth hormones, thyroid hormones, sex hormones, cortisol, and prolactin. Neuroendocrine blood tests can compare these hormone levels to norms to objectively evidence this injury.
Neuro-optometric testing
The eyes are a window into the functioning of the brain. It is estimated that up to 80% of our perception, learning, cognition and activities are mediated at least to some extent through vision. (NeuroRehabilitation 27 (2010) 215-216.) There is an extremely high incidence (greater than 50%) of visual and visual-cognitive disorders in traumatic brain injury. (Ibid.) Neuro-optometric testing can objectively demonstrate these abnormalities, including:
Visual evoked potentials (VEP): Brain injuries can reduce the speed of visual processing. In this test electrodes are placed on the head of the client to record the speed of light stimulus responses as electrical signals travel from the eyes to the visual cortex. These responses can be compared to standardized norms in graph form;
Computerized/automated visual field test: Brain injuries can affect the client’s field of vision. In this test the client pushes a button when they observe the light projected in the visual field, the missed targets are then plotted on a chart to show the client’s defects in the visual field. This test includes reliability measures;
Ocular cyclotorsion: Brain injuries can cause a slight tilt or rotation of the eyes relative to their orbits, which can be objectively measured on an image of the client’s retina and compared to norms.
Vestibular and balance testing
Brain injuries may cause damage to the central nervous system, which impairs your client’s vestibular and balance system. There are a number of objective and computerized tests that can objectively demonstrate these abnormalities, including:
Computerized dynamic posturography (CDP): A virtual reality system is used while your client stands on a moving platform to assess your client’s balance compared to norms;
Videonystagmography (VNG): Brain injuries may cause rapid involuntary eye movements called nystagmus, which may occur all the time or with specific eye movements. VNG testing involves the use of goggles that display moving dots or flashes of light. The goggles track and record eye movements to identify objective evidence of nystagmus;
Vestibular-evoked myogenic potential test (VEMP): Brain injuries may injure the nerve pathways associated with the vestibular system. VEMP involves the placement of electrodes on the head and neck to measure the nerve’s response to auditory stimuli;
Rotational vestibular test (RVT): The test involves placing your client in a rotating chair in a dark room with beams of light projected on the walls, recording their response to stimuli, and comparing it to norms;
Video head impulse test (vHIT): This test objectively measures the eye rotation response to an abrupt head rotation and compares it to norms.
Neuropsychological and speech pathology testing and measures
Brain injuries can create cognitive deficits in areas such as memory, attention, language, and problem-solving. These deficits can be demonstrated through extensive neuropsychological testing and speech pathology testing in multiple domains. Since this testing relies on your client’s responses, it is not purely objective. However, validity measures can give this testing enhanced objectivity. Furthermore, this testing can be critical to determine the extent of cognitive deficits, future treatment, and life care plan needs.
Final thoughts
This list is by no means comprehensive, and there are other objective tests that can evidence your client’s brain injury. Furthermore, every brain injury is unique in its severity and involves different structures of the brain, so it is expected that your brain-injured client will have positive results for some tests and not others. However, by utilizing a variety of multi-disciplinary and objective test methods, it is possible to overwhelmingly refute defendant’s “no objective evidence” claims with highly persuasive scans, graphs and charts that objectively evidence your client’s brain injury. Such evidence will also graphically demonstrate the nature and extent of your client’s cognitive limitations and future needs.
Defendant’s denial of your client’s brain injury cannot credibly withstand the astronomical odds of all these multi-disciplinary and objective testing methods being somehow wrong – facilitating settlement or the loss of defense credibility at trial.
Robert Jarchi

Robert Jarchi won over nine figures in 100 days this year alone for his clients, and has won awards for much more over his 23-year career as an attorney and partner at Greene, Broillet & Wheeler. Rob’s practice includes brain injuries, toxic torts, burn injuries, and wrongful death matters.
Copyright ©
2026
by the author.
For reprint permission, contact the publisher: Advocate Magazine